Up To Date Biomedical Instrumentation MCQs – Oximeters ( Biomedical Instrumentation ) MCQs
Latest Biomedical Instrumentation MCQs
By practicing these MCQs of Oximeters ( Biomedical Instrumentation ) MCQs – Latest Competitive MCQs , an individual for exams performs better than before. This post comprising of objective questions and answers related to “ Oximeters ( Biomedical Instrumentation ) Mcqs “. As wise people believe “Perfect Practice make a Man Perfect”. It is therefore practice these mcqs of Biomedical Instrumentation to approach the success. Tab this page to check ” Oximeters ( Biomedical Instrumentation )” for the preparation of competitive mcqs, FPSC mcqs, PPSC mcqs, SPSC mcqs, KPPSC mcqs, AJKPSC mcqs, BPSC mcqs, NTS mcqs, PTS mcqs, OTS mcqs, Atomic Energy mcqs, Pak Army mcqs, Pak Navy mcqs, CTS mcqs, ETEA mcqs and others.
Biomedical Instrumentation MCQs – Oximeters ( Biomedical Instrumentation ) MCQs
The most occurred mcqs of Oximeters ( ) in past papers. Past papers of Oximeters ( Biomedical Instrumentation ) Mcqs. Past papers of Oximeters ( Biomedical Instrumentation ) Mcqs . Mcqs are the necessary part of any competitive / job related exams. The Mcqs having specific numbers in any written test. It is therefore everyone have to learn / remember the related Oximeters ( Biomedical Instrumentation ) Mcqs. The Important series of Oximeters ( Biomedical Instrumentation ) Mcqs are given below:
Oximeters
1. Blood flow detectors based on Doppler shift start detecting foetal pulses as early as in which week of pregnancy?
a) tenth
b) eleventh
c) twelfth
d) ninth
Answer: b
Explanation: Blood flow detectors based on ultrasonic Doppler shift can detect foetal pulse as early as the tenth week of pregnancy and in nearly all cases by the twelfth week. At about 20 weeks it is possible to detect multiple pregnancies especially if two instruments are used together and the pulse rates compared. Intrauterine death of the foetus can also be diagnosed.
2. When it is possible to detect multiple pregnancies?
a) 10th week
b) 12th week
c) 15th week
d) 20th week
Answer: d
Explanation: Blood flow detectors based on ultrasonic Doppler shift can detect foetal pulse as early as the tenth week of pregnancy and in nearly all cases by the twelfth week. At about 20 weeks it is possible to detect multiple pregnancies especially if two instruments are used together and the pulse rates compared. Intrauterine death of the foetus can also be diagnosed.
3. Which of the following is the most reliable method for detecting FHR pattern?
a) Abdominal foetal electrocardiogram
b) Foetal phonocardiogram
c) Ultrasound technique
d) Foetal ECG with scalp electrode
Answer: c
Explanation: We can hear the signal through a loudspeaker with a scarce chance of failing to recognize any beat, but a simple electronic circuit may fail to trigger from this signal. Still, the ultrasound Doppler shift method is more practical and easy to use during labour. It is currently the most reliable method for detecting the FHR pattern that is interpretable.
4. Signal processing for FHR determination can be based either on detecting the foetal heart valve motion or on detecting the heart wall motion in Abdominal foetal electrocardiogram technique.
a) True
b) False
Answer: b
Explanation: False, Signal processing for FHR determination can be based either on detecting the foetal heart valve motion or on detecting the heart wall motion in Ultrasound technique as The heart valve motion detection technique is based on the distinct ultrasound frequency shift produced by the fast opening and closing of the heart valves. The technique, however, requires that the ultrasound beam must be directed against the relatively small heart valves involving a longer search period and frequent repositioning of the transducer. Therefore, it is not preferred for continuous monitoring applications.
5. What is maximum ultrasound intensity of narrow beam transducer?
a) 15 mW/cm2
b) 20 mW/cm2
c) 25 mW/cm2
d) 30 mW/cm2
Answer: c
Explanation: The narrow beam transducer uses a single ultrasound transmitter/receiver piezo-electric crystal pair. The maximum ultrasound intensity is generally kept below 25 mW/cm2. The typical transducer diameter is 25 mm. The narrow beam transducer is very sensitive and produces a good trigger signal for instantaneous heart rate determination.
6. What is the diameter of a narrow beam transducer?
a) 15 mm
b) 20 mm
c) 25 mm
d) 30 mm
Answer: c
Explanation: The narrow beam transducer uses a single ultrasound transmitter/receiver piezo-electric crystal pair. The maximum ultrasound intensity is generally kept below 25 mW/cm2. The typical transducer diameter is 25 mm. The narrow beam transducer is very sensitive and produces a good trigger signal for instantaneous heart rate determination.
7. What is used to detect foetal heart movements in broad beam transducer?
a) Quartz crystal
b) Piezo electric crystal
c) Topaz crystal
d) Berlinite crystal
Answer: b
Explanation: The broad beam transducers are available in many configurations. The transducers comprise a number of piezo-electric crystals mounted in such a way as to be able to detect foetal heart movements over a wider area.
8. The narrow beam transducer is very sensitive and produces a good trigger signal for instantaneous heart rate determination.
a) True
b) False
Answer: a
Explanation: True, The narrow beam transducer is very sensitive and produces a good trigger signal for instantaneous heart rate determination because it takes time to detect a good signal and, therefore, frequent transducer repositioning is necessary.
9. Which of the following transducer is used to detect foetal heart movements over a wider area?
a) piezo-electric
b) ultrasonic
c) array
d) pressure
Answer: a
Explanation: The broad beam transducers are available in many configurations. The transducers comprise a number of piezo-electric crystals mounted in such a way as to be able to detect foetal heart movements over a wider area.
10. Which transducer is arranged in the shape of a clover leaf so that it provides a large area of illumination?
a) piezo-electric
b) ultrasonic
c) array
d) pressure
Answer: b
Explanation: The ultrasonic transducer is arranged in the shape of a clover-leaf so that it provides a large area of ultrasonic illumination which allows the monitoring considerable lateral and descending foetal motion before requiring repositioning. The transducer housing is flexible to permit it to follow the contour of the abdomen regardless of shape changes with contractions.
11. The array transducer housing is flexible to permit it to follow the contour of the abdomen regardless of shape changes with contractions.
a) True
b) False
Answer: b
Explanation: False, the ultrasonic transducer is arranged in the shape of a clover-leaf so that it provides a large area of ultrasonic illumination which allows the monitoring considerable lateral and descending foetal motion before requiring repositioning. The ultrasonic transducer housing is flexible to permit it to follow the contour of the abdomen regardless of shape changes with contractions.
12. At what angle divergent beam is transmitted by a crystal in array transducer?
a) 10°
b) 20°
c) 30°
d) 40°
Answer: d
Explanation: An alternative arrangement is the array transducer which has one transmitter and six peripheral ceramic receiving crystals. The transmitting crystal emits a 40° divergent beam so that at 10 cm from the skin surface the beam covers an area of approximately 10 cm diameter.
13. The transmitting crystal emits 40° divergent beam so that the beam covers an area of approximately _____ cm diameter.
a) 10
b) 20
c) 30
d) 40
Answer: a
Explanation: An alternative arrangement is the array transducer which has one transmitter and six peripheral ceramic receiving crystals. The transmitting crystal emits a 40° divergent beam so that at 10 cm from the skin surface the beam covers an area of approximately 10 cm diameter.
14. What is the diameter of an array transducer?
a) 2
b) 4
c) 6
d) 8
Answer: c
Explanation: The transmitting crystal emits a 40° divergent beam so that at 10 cm from the skin surface the beam covers an area of approximately 10 cm diameter. This construction ensures continuous recording of the foetal heart activity without the need to reposition the transducer which is otherwise necessitated due to normal foetal movement. The transducer has a diameter of 6 cm and can be held in place either by a simple buckle or a stretch belt.
15. The array transducer can be held in place by a simple buckle.
a) True
b) False
Answer: a
Explanation: True, the transmitting crystal emits a 40° divergent beam so that at 10 cm from the skin surface the beam covers an area of approximately 10 cm diameter. This construction ensures continuous recording of the foetal heart activity without the need to reposition the transducer which is otherwise necessitated due to normal foetal movement. The transducer has a diameter of 6 cm and can be held in place either by a simple buckle or a stretch belt.
Ear Oximeter
1. What is intrauterine pressure during the expulsion period?
a) 130 mm Hg
b) 140 mm Hg
c) 150 mm Hg
d) 160 mm Hg
Answer: c
Explanation: During labour, the uterus muscle starts contractions of increasing intensity in a bid to expel out the child. The intrauterine pressure can reach values of 150 mmHg or more during the expulsion period. However, a normal patient in spontaneous active labour will demonstrate uterine contractions occurring at intervals of three to five minutes, with a duration of 30 to 70 s and a peak intensity of 50 to 75 mmHg.
2. What is the interval of uterine contractions in a normal patient in spontaneous active labour?
a) 1 to 3 minutes
b) 3 to 5 minutes
c) 5 to 7 minutes
d) 7 to 9 minutes
Answer: c
Explanation: During labour, the uterus muscle starts contractions of increasing intensity in a bid to expel out the child. The intrauterine pressure can reach values of 150 mmHg or more during the expulsion period. However, a normal patient in spontaneous active labour will demonstrate uterine contractions occurring at intervals of three to five minutes, with a duration of 30 to 70 s and a peak intensity of 50 to 75 mmHg.
3. What is the duration of uterine contractions in a normal patient in spontaneous active labour?
a) 0 to 30 s
b) 30 to 70 s
c) 80 to 100 s
d) 110 to 150 s
Answer: b
Explanation: During labour, the uterus muscle starts contractions of increasing intensity in a bid to expel out the child. The intrauterine pressure can reach values of 150 mmHg or more during the expulsion period. However, a normal patient in spontaneous active labour will demonstrate uterine contractions occurring at intervals of three to five minutes, with a duration of 30 to 70 s and a peak intensity of 50 to 75 mmHg.
4. The toco-transducers are temperature sensitive.
a) True
b) False
Answer: b
Explanation: False, the toco-transducers are location sensitive. They should be placed over the fundus where there is maximum motion with the contractions. The toco-tonometer transducer cannot be used in the same place as the foetal heart rate detector, thus the patient must have two transducers on her abdomen.
5. What is the peak intensity of uterine contractions in a normal patient in spontaneous active labour?
a) 0 to 35 mm Hg
b) 50 to 75 mm Hg
c) 90 to 120 mm Hg
d) 120 to 150 mm Hg
Answer: b
Explanation: During labour, the uterus muscle starts contractions of increasing intensity in a bid to expel out the child. The intrauterine pressure can reach values of 150 mmHg or more during the expulsion period. However, a normal patient in spontaneous active labour will demonstrate uterine contractions occurring at intervals of three to five minutes, with a duration of 30 to 70 s and a peak intensity of 50 to 75 mmHg.
6. What are labour-activity transducers?
a) temperature transducer
b) ultrasonic transducer
c) pressure transducer
d) piezoelectric transducer
Answer: c
Explanation: The labour-activity transducers are pressure transducers that drive circuits for obtaining an electrical indication of pressure by conventional means. The pressure channel on the recorder is provided with a positioning control. This is done because the baseline is affected by the static pressure on the transducer that results from the tension on the belt holding the transducer in place.
7. What is used to convert the movement of transducer due to an increase of tension in uterus into an electric signal?
a) AC Amplifier
b) Strain guage
c) Synchronous detector
d) piezoelectric crystal
Answer: b
Explanation: The transducer carries a protruding tip which is pressed to the mother’s abdomen with a light force to ensure an effective coupling. The protruding surface of the transducer is displaced as the tension in the uterus increases. This movement is converted into an electrical signal by a strain gauge in the transducer housing. The abdominal transducer provides a reliable indication of the occurrence frequency, duration and relative intensity of the contraction.
8. The narrow beam transducer permits the operator to position the baseline on the zero-level line of recording chart.
a) True
b) False
Answer: b
Explanation: False, the labour-activity transducers are pressure transducers that drive circuits for obtaining an electrical indication of pressure by conventional means. The pressure channel on the recorder is provided with a positioning control. This is done because the baseline is affected by the static pressure on the transducer that results from the tension on the belt holding the transducer in place. The control permits the operator to position the baseline on the zero-level line of the recording chart.
9. In external toco-tonometry, movement of _____ may be superimposed on labour activity.
a) heart
b) eye
c) foetus
d) muscle
Answer: c
Explanation: In external toco-tonometry, movement of the foetus may be superimposed on the labour activity curve. Stress imposed on the foetal circulatory system by the uterine contractions, foetal movements or other factors are seen in the response of the foetal heart to these stimuli and are studied in the correct time relationship.
10. What is measured in the internal method using fluid-filled catheter?
a) IUP
b) ECG
c) IUC
d) EMG
Answer: a
Explanation: The internal method measures intra-uterine pressure (IUP) via a fluid-filled catheter. The catheter is inserted into the uterus through a guide after the rupture of the foetal membranes. After allowing free flow of amniotic fluid to ensure correct placement, the distal end of the catheter is usually attached to a pressure transducer of the type used for cardiac studies.
11. What is the range of Instantaneous beat to beat rate digitally displayed?
a) 0 to 50 bpm
b) 50 to 210 bpm
c) 210 to 350 bpm
d) 350 to 410 bpm
Answer: b
Explanation: Instantaneous “beat-to-beat” rate is displayed on a calibrated linear scale or digitally displayed with a range from 50 to 210 bpm. A two-channel chart recorder is incorporated in instruments used for monitoring labour activity. One channel records FHR on a calibrated chart in beats per minute (50–210 bpm) while the other channel is used for recording uterine contractions calibrated 0-100 mmHg.
12. A _______ channel chart recorder is incorporated in instruments used for monitoring labour activity.
a) one
b) two
c) three
d) four
Answer: b
Explanation: Instantaneous “beat-to-beat” rate is displayed on a calibrated linear scale or digitally displayed with a range from 50 to 210 bpm. A two-channel chart recorder is incorporated in instruments used for monitoring labour activity. One channel records FHR on a calibrated chart in beats per minute (50–210 bpm) while the other channel is used for recording uterine contractions calibrated 0-100 mmHg.
Foetal Monitoring Instruments MCQs
13. What is the standard chart speed?
a) 2 cm/min
b) 3 cm/min
c) 4 cm/min
d) 5 cm/min
Answer: a
Explanation: A two-channel chart recorder is incorporated in instruments used for monitoring labour activity. One channel records FHR on a calibrated chart in beats per minute (50–210 bpm) while the other channel is used for recording uterine contractions calibrated 0-100 mmHg. The standard chart speed is usually 1 or 2 cm/min.
14. In two-channel chart recorder, FHR is recorded on a calibrated chart in ________
a) cm/min
b) m/min
c) beats/min
d) pulses/min
Answer: c
Explanation: A two-channel chart recorder is incorporated in instruments used for monitoring labour activity. One channel records FHR on a calibrated chart in beats per minute (50–210 bpm) while the other channel is used for recording uterine contractions calibrated 0-100 mmHg. The standard chart speed is usually 1 or 2 cm/min.
15. Uterine contractions are calibrated in range of ______ in two-channel chart recorder.
a) 0-100 mm Hg
b) 100-200 mm Hg
c) 200-300 mm Hg
d) 300-400 mm Hg
Answer: a
Explanation: A two-channel chart recorder is incorporated in instruments used for monitoring labour activity. One channel records FHR on a calibrated chart in beats per minute (50–210 bpm) while the other channel is used for recording uterine contractions calibrated 0-100 mmHg. The standard chart speed is usually 1 or 2 cm/min.
Pulse Oximeter
1. _____ is non-invasive method allowing the monitoring of the saturation of a patient’s hemoglobin.
a) Ear Oximetry
b) Pulse Oximetry
c) Skin-Reflectance Oximetry
d) Intravascular Oximetry
Answer: b
Explanation: Pulse oximetry is a non-invasive method allowing the monitoring of the saturation of a patient’s hemoglobin. A pulse oximeter shows the percentage of arterial hemoglobin in the oxyhemoglobin (HbO2) and hemoglobin (Hb). These observations:
A = -logT = log I0/I =ɛDC.
2. A = log I0/I,where I0 is_____
a) Incident light Intensity
b) Transmitted light Intensity
c) Extinction coefficient
d) Concentration
Answer: a
Explanation: A pulse oximeter shows the percentage of arterial hemoglobin in the oxyhemoglobin (HbO2) and hemoglobin (Hb). This observation A = -logT = log I0/I = ɛDC where Io and I are incident and transmitted light intensities, e is the extinction coefficient, D is the depth of the absorbing layer and C is concentration.
3. A = ɛDC, where ɛ is _______
a) Incident light Intensity
b) Transmitted light Intensity
c) Extinction coefficient
d) Concentration
Answer: c
Explanation: A pulse oximeter shows the percentage of arterial hemoglobin in the oxyhemoglobin (HbO2) and hemoglobin (Hb). This observation A = -logT = log I0/I = ɛDC where Io and I are incident and transmitted light intensities, e is the extinction coefficient, D is the depth of the absorbing layer and C is concentration.
4. A pulse oximeter shows the percentage of venous hemoglobin in the oxyhemoglobin (HbO2) and hemoglobin (Hb).
a) True
b) False
Answer: b
Explanation: False, pulse oximetry is a non-invasive method allowing the monitoring of the saturation of a patient’s hemoglobin. A pulse oximeter shows the percentage of arterial hemoglobin in the oxyhemoglobin (HbO2) and hemoglobin (Hb). These observations:
A = -logT = log I0/I =ɛDC.
5. What is used as a photodetector in pulse oximetry?
a) Phototransistor
b) Solar cell
c) Photodiode
d) Photographic plates
Answer: c
Explanation: Pulse oximetry is a particularly convenient noninvasive measurement method. Typically it utilizes a pair of small light-emitting diodes (LEDs) facing a photodiode through a translucent part of the patient’s body, usually a fingertip or an earlobe. One LED is red, with a wavelength of 660 nm, and the other is infrared, 905, 910, or 940 nm.
6. What is the wavelength of the red LED in pulse oximetry?
a) 660 nm
b) 740 nm
c) 905 nm
d) 950 nm
Answer: a
Explanation: Pulse oximetry is a particularly convenient noninvasive measurement method. Typically it utilizes a pair of small light-emitting diodes (LEDs) facing a photodiode through a translucent part of the patient’s body, usually a fingertip or an earlobe. One LED is red, with a wavelength of 660 nm, and the other is infrared, 905, 910, or 940 nm.
7. What is the wavelength of infrared LED in pulse oximetry?
a) 660 nm
b) 740 nm
c) 905 nm
d) 950 nm
Answer: c
Explanation: Pulse oximetry is a particularly convenient noninvasive measurement method. Typically it utilizes a pair of small light-emitting diodes (LEDs) facing a photodiode through a translucent part of the patient’s body, usually a fingertip or an earlobe. One LED is red, with a wavelength of 660 nm, and the other is infrared, 905, 910, or 940 nm.
8. A pulse oximeter is useful in any setting where a patients oxygenation is unstable.
a) True
b) False
Answer: a
Explanation: True, pulse oximeter is useful in any setting where a patient’s oxygenation is unstable, including intensive care, operating, recovery, emergency and hospital ward settings, pilots in unpressurized aircraft, for assessment of any patient’s oxygenation, and determining the effectiveness of or need for supplemental oxygen.
9. Portable pulse oximeters are useful for ______ whose oxygen levels may decrease at high altitude.
a) Athlete
b) Swimmer
c) Mountain climber
d) Fisher
Answer: c
Explanation: Portable pulse oximeter is also useful for mountain climbers and athletes whose oxygen levels may decrease at high altitudes or with exercise. Some portable pulse oximeters employ software that charts a patient’s blood oxygen and pulse, serving as a reminder to check blood oxygen levels.
10. ______ is very useful for patients having respiratory or cardiac problems because of their simplicity of use and the ability to provide continuous and immediate oxygen saturation levels.
a) Pulse Oximeter
b) Ear Oximeter
c) Skin Reflactance Oximeter
d) Intravascular Oximeter
Answer: a
Explanation: Because of their simplicity of use and the ability to provide continuous and immediate oxygen saturation values, pulse oximeters are of critical importance in emergency medicine and are also very useful for patients with respiratory or cardiac problems, especially COPD, or for diagnosis of some sleep disorders such as apnea and hypopnea.
Skin Reflectance Oximeters
1. Which module consists of a pair of Perspex plates?
a) The dialyzer module
b) The recorder module
c) The sampling module
d) Heating bath module
Answer: a
Explanation: In analytical chemistry, it is often necessary to remove protein cells to obtain an interference-free analysis. This is accomplished by dialysis in the auto-analyzer. The dialyzer module consists of a pair of perspex plates, the mating surfaces of which are mirror grooved in a continuous channel, which goes in towards the centre, on itself and returns to the outside.
2. The part of the automated system that shown in the figure is ____________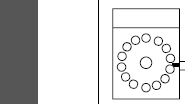
a) Dialyzer
b) Pump
c) Recorder
d) Sampler
Answer: d
Explanation: The automated system consists of a group of modular instruments interconnected together by a manifold system and electrical systems. The sample to be analyzed is introduced into a stream of diluting liquid flowing in the narrow bore of a flexible plastic tube. The stages of the analytical reaction are completed by the successive combination of other flowing streams of liquids with the sample stream, by means of suitably shaped glass functions.
3. In the sampling unit, when it is in its earlier form consisted of a circular turntable carrying around its rim 40 disposable __________ of 2 ml capacity.
a) Polyvinyl cups
b) Polythene cups
c) Polyester cups
d) Polystyrene cups
Answer: d
Explanation: The unit in its earlier form consisted of a circular turntable carrying around its rim 40 disposable polystyrene cups of 2 ml capacity. The sample plate carrying these cups rotates at a predetermined speed. The movement of the turntable is synchronized with the movements of a sampling crook.
4. What is the ratio of the sampling time to wash time?
a) 1:2
b) 3:1
c) 2:1
d) 1:3
Answer: c
Explanation: Between each sampling, the crook enters a receptacle of water or other suitable wash fluid, to reduce cross-contamination of one sample with another. The ratio of sampling time to wash time is normally 2:1.
5. Which of the following is not the part of the manifold?
a) Transmission tubing
b) Pump tubes
c) Platter
d) Plastic tubes
Answer: d
Explanation: A manifold mainly consists of a platter, pump tubes, coils, transmission tubing, fittings and connections. A separate manifold is required for each determination and the change can be effected within a few minutes. The pump tubing and the connected coils are placed on a manifold platter, which keeps them in proper order for each test.
6. Which of the following is not the type of tubing?
a) Acidflex tubing
b) Glass tubing
c) Polypropylene tubing
d) Tygon
Answer: c
Explanation: Several other tubes are required to introduce reagents and to transport the specimen from one module to another. There are five types of such tubings. They are of varying sizes and are to be selected according to the requirements. These are standard transmission tubing (Tygon), solvaflex tubing, acidflex tubing, polyethylene tubing and glass tubing.
7. There are two types of coils employed in the system, which are ____
a) Tygon coils and mixing coils
b) Mixing coils and tubing coils
c) Delay coils and tygon coils
d) Mixing coils and delay coils
Answer: d
Explanation: Two types of coils are employed in the system—mixing coils and delay coils. Coils are glass spirals of critical dimensions, in which the mixing liquids are inverted several times, so that complete mixing can result. Mixing coils are used to mix the sample and/or reagents. Delay coils are employed when a specimen must be delayed for the completion of a chemical reaction before reaching the colorimeter.
8. In phasing, if the cholesterol stream arrives at Y time, albumin must arrive at ______
a) Y + 5 s
b) Y + 10 s
c) Y + 15 s
d) Y + 20 s
Answer: c
Explanation: With 12 tests to be recorded on each sample and a sampling rate of 60 samples per hour, it follows that 5 s are allowed to record each steady state plateau. The reaction streams in the 12 channels and up to four blank channels must, therefore, be phased to arrive at the colorimeter in waves 5 s apart. For example, if the cholesterol stream arrives at X time, calcium must arrive at X + 5 s, total protein at X + 10 s, albumin at X + 15 s, etc.
9. Which coils are used to permit the channels to enter the calorimeter in the proper sequence?
a) Mixing coils
b) Delay coils
c) Solvaflex coils
d) Phasing coils
Answer: d
Explanation: In order to ensure a proper sequencing for the presentation of results, a number of devices have been provided to make this adjustment an extremely simple operation. Phasing coils are used to permit the channels to enter the colorimeter in the proper sequence.
Intravascular Oximeters
1. What is the amount of blood in the average adult?
a) 5-10 liters
b) 10-15 liters
c) 5-6 liters
d) 5-15 liters
Answer: c
Explanation: The blood constitutes 5–10% of the total body weight and in the average adult, it amounts to 5–6 l. Blood consists of corpuscles suspended in a fluid called plasma in the proportion of 45 parts of corpuscles (cells) to 55 parts of plasma.
2. Which of the following is not the type of blood cell?
a) Erythrocytes
b) Thrombocytes
c) Leukocytes
d) Eosinocytes
Answer: d
Explanation: The percentage of cells in the blood is called the haematocrit value or packed cell volume (PCV). The majority of the corpuscles in the blood are red blood cells (erythrocytes), others being white blood cells (leucocytes or Leukocytes) and platelets (thrombocytes).
3. Which of the following is the Red Blood Cells?
a) Erythrocytes
b) Leukocytes
c) Basophils
d) Monocytes
Answer: a
Explanation: Erythrocytes (Red Blood Cells): Red blood cells have the form of a bi-concave disc with a mean diameter of about 7.5 m and thickness of about 1.7 m. The mean surface area of the cell is about 134mm2. There are about 5.5 million of them in every cubic millimetre of blood in men and nearly 5 million in women.
4. The normal red cell lasts approximately ______ before it is destroyed.
a) 90 days
b) 210 days
c) 120 days
d) 60 days
Answer: c
Explanation: In the whole body, there are about 25 billion erythrocytes and they are constantly being destroyed and replaced at a rate of about 9000 million per hour. The normal red cell lasts approximately 120 days before it is destroyed.
5. Who is responsible for carrying oxygen from the lungs to the tissues and carbon dioxide from the tissues to the lungs?
a) Basophils
b) Eosinophils
c) RBC
d) Thrombocytes
Answer: c
Explanation: The erythrocytes have no nucleus. They are responsible for carrying oxygen from the lungs to the tissues and carbon dioxide from the tissues to the lungs. Anaemia (reduction in the oxygen carrying capacity of blood) can develop from a change in the number, volume or Hb concentration of erythrocytes, caused by bone marrow dysfunction resulting in the poor production rate of RBCs.
6. The main two types of leukocytes are ____________
a) The neutrophils and the thrombophils
b) The lymphocytes and the neutrophils
c) The neutrophils and the monophils
d) The lymphocytes and the monophils
Answer: b
Explanation: Leucocytes form the defence mechanism of the body against infection. They are of two main types: the neutrophils and the lymphocytes. Neutrophils ingest bacteria and lymphocytes are concerned with an immunological response.
7. ______ play an important role in the blood coagulation process.
a) Platelets
b) Leukocytes
c) RBC
d) Neutrophils
Answer: a
Explanation: Platelets are usually tiny, round, oblong or irregularly shaped cells of the blood with an average diameter of approximately 2 m. They play an important role in the blood coagulation process. There are usually 250,000–750,000 platelets in every cubic mm of blood.
8. Which of the following is not the method of cell counting?
a) Microscopic method
b) Electrical conductivity method
c) Automatic optical method
d) Electroscopic method
Answer: d
Explanation: There are three methods of cell counting: i) Microscopic method, ii) Automatic optical method, iii) Electrical conductivity method.
9. What is the difference of measuring accuracy between microscopic counting and electronic counters?
a) + or – 20 %
b) + or – 17%
c) + or – 3%
d) + or – 23%
Answer: b
Explanation: Agoston and Zillich (1971) compared the results of microscopic counting with those made by electronic counters. It may be observed that instead of the + 0r – 20% measuring accuracy in microscopic counting, the electronic counters can provide an accuracy of + or – 3%.
10. What is the ratio of a sample of red blood cells in dilute blood?
a) 500:1
b) 50000:1
c) 1:500
d) 1:50000
Answer: d
Explanation: The method is based on collecting scattered light from the blood cells and converting them into electrical pulses for counting. A sample of dilute blood (1:500 for white cells and 1:50,000 for red cells) is taken in a glass container. It is drawn through a counting chamber in which the blood stream is reduced in cross-section by a concentric high velocity liquid sheath.
11. The instrument of an optical method of counting cells, that require about _____ of blood sample.
a) 100 ml
b) 1 liter
c) 1 ml
d) 10 ml
Answer: c
Explanation: Instruments based on optical technique take about 30 s for completing the count. An accuracy of 2% is attainable. The instruments require about 1 ml of the blood sample.
12. 1 f/l = ____
a) 1018
b) 1015
c) 10-18
d) 10-15
Answer: d
Explanation: f/l = Femolitres
1f/l = 10-15.
13. _______ will be calculated if the value of PCV and Hb per deciliters are known.
a) MCV
b) MCHC
c) MCH
d) PCT
Answer: b
Explanation: It can be calculated if PCV and Hb per dl are known. For example, if PCV is 0.45 and there are 15 g Hb per dl of blood, then
MCHC = (15 /0.45) g/dl
= 33.3 g/dl.
14. PDW index is related to the size range covered by those platelets lying between _______ and _______ percentile.
a) 20th and 84th percentile
b) 16th and 20th percentile
c) 16th and 84th percentile
d) 20th and 80th percentile
Answer: c
Explanation: Platelet Distribution Width (PDW): This index is related to the size range covered by those platelets lying between the sixteenth and eighty fourth percentile. This is the conventional geometric standard deviation of the mean platelet size and is derived from the distribution curve based on the data in a 64-channel pulse height analyzer.
15. Instruments based on the automatic optical technique take about _____ for completing the count blood cells.
a) 30 sec
b) 120 sec
c) 60 sec
d) 90 sec
Answer: a
Explanation: Instruments based on this automatic optical technique take about 30 s for completing the count. An accuracy of 2% is attainable. The instruments require about 1 ml of the blood sample.
